What Does A Nurse Case Manager Do For An Insurance Company
I like the position pretty well and have been at it for 2 years now. Anyway at the beginning I.
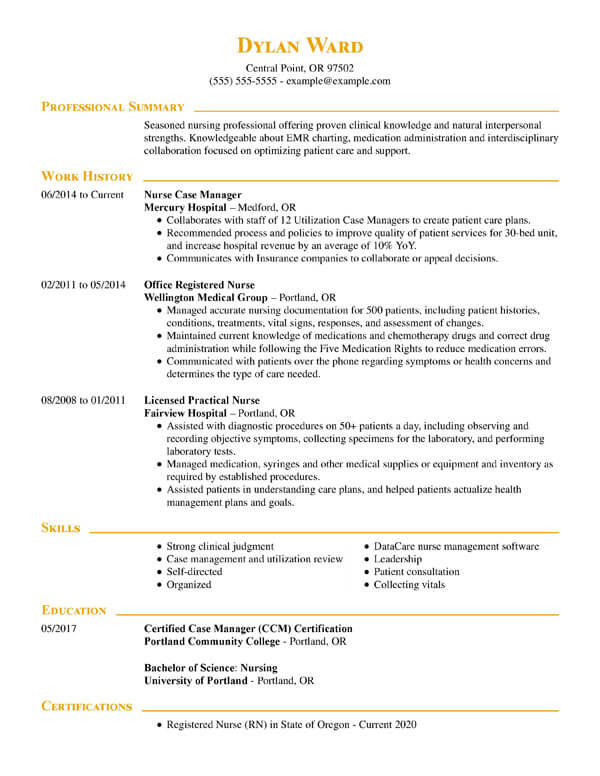
 Case Manager Resume Example Guide 2021 Zipjob
Case Manager Resume Example Guide 2021 Zipjob
This Nurse Case Manager is basically another adjuster on your case and reports to the people who pay hisher paychecks.

What does a nurse case manager do for an insurance company. The work comp insurance company. The role of the nurse case manager is to monitor your care and report back to the insurance adjuster. A case manager is a specialized Registered Nurse RN that works with patients and providers to determine the specific care that is required and the best options for that care.
She is not attending your appointments to help you get better but rather for the insurance company that wants to cut off your medical care and benefits. At the moment I work as an RN case manager. I really wanted to make a difference from a different perspective other than at the bedside.
This estimate is based upon 91 Aetna RN Case Manager salary reports provided by employees or estimated based upon statistical methods. I started off very enthused and pumped as this was a new venture for me. While they do provide the insurance company with relevant information about a patients condition and medical treatment they should not advocate against the patient during settlement negotiations or otherwise perform investigative activity on the insurance companys behalf.
The typical Aetna RN Case Manager salary is 77242. The nurse case managers job is to keep everyone updated and on task. Many times there may be underlying pressure on the doctor to force an injured worker back to work too quickly or to suggest cheaper medical treatment as opposed to what a physician may truly want to do.
Its case management program involves trained nurse case managers offering free service and support helping members manage their benefits arrange care and find resources. Never forget that no matter how kind they are to you. In a hospital a nurse case manager is in charge of coordinating care plans and health services upon discharge from the hospital.
In addition the case manager coordinates the services of other members of the healthcare team and caregivers communicates with the health insurance company communicates with the patients physician and supervises visiting nurses and other home health aides who provide support. They can work for healthcare practitioners hospitals or insurance companies. Under the rule it is not clear whether the nurse case manager works directly for the insurance company or not.
I am a Telephonic Nurse Case Manager in Workers Compensation for a well known Insurance Company. A registered nurse case manager is a registered nurse who integrates the needs of the individual patient with medical services and insurance companies. RN Case Manager salaries at Aetna can range from 64776 - 92920.
Through a collaboration with multiple specialties case managers ensure the patient is receiving quality medical care. So heres the good bad and ugly on nurse case managersplus a review of your most important rights. Unfortunately it is not as clear what the nurse case managers job is when the insurance company uses Rule 2002 to hire a case manager.
In 2009 I chose to become an RN Case Manager RN CM for an insurance company. If you signed a form for your case that allows the Nurse Case Manager to communicate with your doctor then it is allowed. Generally he or she must also act as an advocate for the patient with insurance companies in order to ensure home health care medical equipment and rehabilitation services are covered after discharge.
The registered nurse case manager collaborates with all professionals who provide care for patients and ensure that all available resources are considered in. So I recently started a nurse case manager job at an insurance company. I received a call from Blue Cross Blue Shield of MI offering me an interview for a Case Manager position with them.
For you they are supposed to facilitate coordinate and manage your care. The nurse educates injured workers on proper care mediates between the employer and their worker moderates the physicians care plan and negotiates with the employer and insurer to get the best care outcome while saving costs. Legally the nurse case managers primary concern is supposed to be your recovery and return to work.
I am going to sit for the CCM exam this August. RN CMs help members learn more about their conditions and medications address symptoms assist with contacting the provider and provide information on general health and lifestyle factors. Theoretically nurse case managers work independently of the insurance company.
Apply to Case Manager Registered Nurse Case Manager Senior Case Manager and more. The role of the nurse case manager is as an agent for the insurance company not a medical provider.
 Introduction To The Case Management Body Of Knowledge Ccmc S Case Management Body Of Knowledge Cmbok
Introduction To The Case Management Body Of Knowledge Ccmc S Case Management Body Of Knowledge Cmbok
 Rn Case Manager Resume Samples Qwikresume
Rn Case Manager Resume Samples Qwikresume
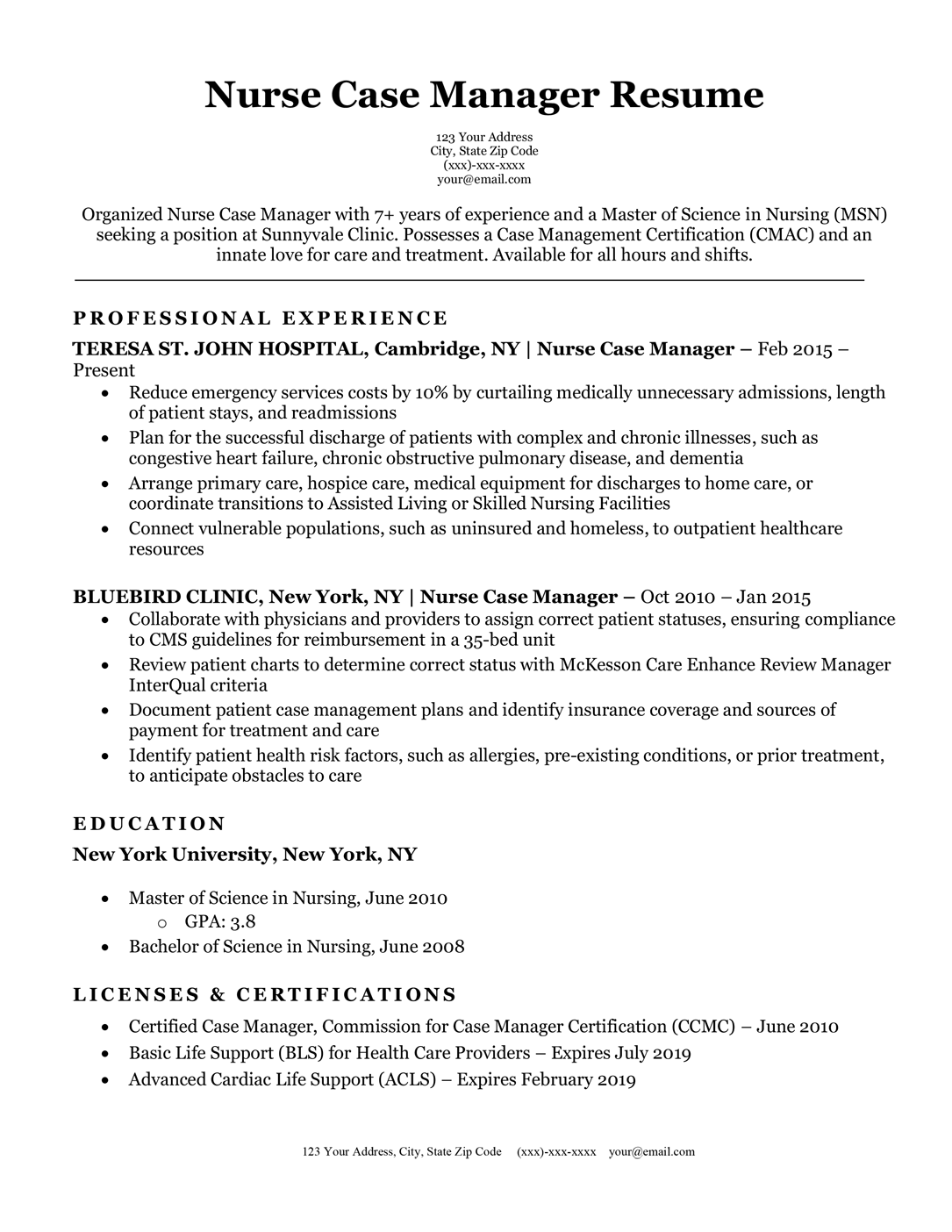 Nurse Case Manager Resume Sample Resume Companion
Nurse Case Manager Resume Sample Resume Companion
 Rn Case Manager Salary And Job Outlook Nursejournal Org
Rn Case Manager Salary And Job Outlook Nursejournal Org

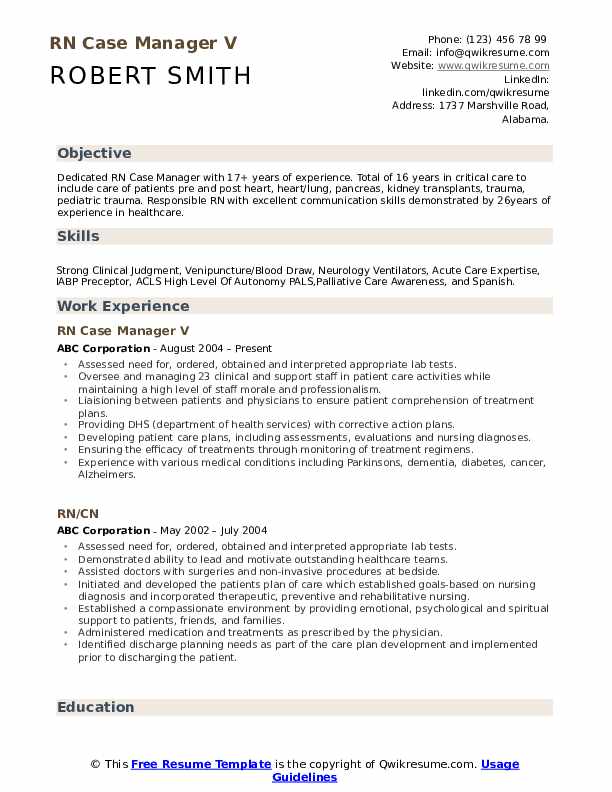 Rn Case Manager Resume Samples Qwikresume
Rn Case Manager Resume Samples Qwikresume
 Introduction To The Case Management Body Of Knowledge Ccmc S Case Management Body Of Knowledge Cmbok
Introduction To The Case Management Body Of Knowledge Ccmc S Case Management Body Of Knowledge Cmbok
 Case Manager Resume Example Guide 2021 Zipjob
Case Manager Resume Example Guide 2021 Zipjob
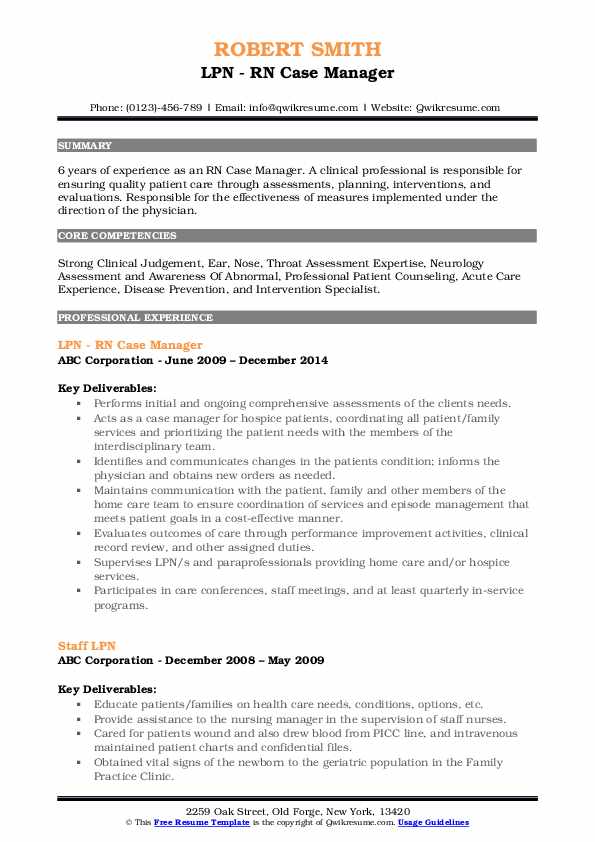 Rn Case Manager Resume Samples Qwikresume
Rn Case Manager Resume Samples Qwikresume
 Nurse Case Manager Registerednursing Org
Nurse Case Manager Registerednursing Org
 Rn Case Manager Resume Samples Qwikresume
Rn Case Manager Resume Samples Qwikresume
 Rn Case Manager Resume Samples Qwikresume
Rn Case Manager Resume Samples Qwikresume
 What Is A Nurse Case Officer During A Workers Comp Case Jebaily Law
What Is A Nurse Case Officer During A Workers Comp Case Jebaily Law
 5 Steps To Becoming An Rn Case Manager Salary Requirements
5 Steps To Becoming An Rn Case Manager Salary Requirements
 Rn Case Manager Resume Samples Qwikresume
Rn Case Manager Resume Samples Qwikresume
 What Is A Nurse Case Officer During A Workers Comp Case Jebaily Law
What Is A Nurse Case Officer During A Workers Comp Case Jebaily Law
 What Does A Case Management Nurse Do
What Does A Case Management Nurse Do
 Professional Nursing Resume Examples Myperfectresume
Professional Nursing Resume Examples Myperfectresume

Post a Comment for "What Does A Nurse Case Manager Do For An Insurance Company"